Table of Contents
Message from the Ombudsman
I am pleased to publish Continuum of Care: A Journey from Home to Long Term Care. It is a report that considers current challenges faced by Veterans as they age and/or require more care, and it makes recommendations to address challenges Veterans encounter along the continuum of care journey: at home, in assisted living and in long term care (LTC).
This report is the fourth in a series and follows three reviews my Office published in 2013 and 2014 on the different aspects of the continuum of care. First we conducted two reviews of Veterans Affairs Canada’s (VAC’s) main programs that provide continuum of care support: the LTC Program and the Veterans Independence Program (VIP). These reviews evaluated the programs based on the criteria of eligibility, accessibility, and cost. A third review followed, which explored the option of assisted living for Veterans who find themselves no longer able to stay at home but not yet ready for LTC.
This report makes seven recommendations which I encourage the Minister of Veterans Affairs and Veterans Affairs Canada to implement within two years of the date of publication. I will continue to monitor VAC’s progress to ensure the best possible outcomes for those who served.
Guy Parent
Veterans Ombudsman
Veterans Ombudsman’s Mandate
The Office of the Veterans Ombudsman (OVO), created by Order in Council, works to ensure that Veterans, serving members of the Canadian Armed Forces (CAF) and the Royal Canadian Mounted Police (RCMP), as well as other clients of VAC, are treated respectfully, in accordance with the Veterans Bill of Rights, and receive the services and benefits that they require in a fair, timely and efficient manner.
The Veterans Ombudsman is an independent and impartial officer who is committed to ensuring that Veterans and other clients of VAC are treated fairly. The Veterans Ombudsman measures fairness in terms of: adequacy, sufficiency and accessibility.
The OVO addresses complaints, emerging and systemic issues related to programs and services provided or administered by VAC, as well as systemic issues related to the Veterans Review and Appeal Board.
Veterans Bill of Rights
The Veterans Bill of Rights applies to all clients of Veterans Affairs. It states:
“You have the right to:
- Be treated with respect, dignity, fairness and courtesy.
- Take part in discussions that involve you and your family.
- Have someone with you for support when you deal with Veterans Affairs.
- Receive clear, easy-to-understand information about our programs and services, in English or French, as set out in the Official Languages Act.
- Have your privacy protected as set out in the Privacy Act.
- Receive benefits and services as set out in our published service standards and to know your appeal rights.
You have the right to make a complaint and have the matter looked into if you feel that any of your rights have not been upheld.”
Executive Summary
The purpose of this report is to: highlight the issues identified in the initial three reviews, as well as in other research; make recommendations to address gaps identified in three key areas across the continuum of care (care at home, assisted living, and LTC); and, provide an update on the current context related to the continuum of care.
Key findings of the report:
- While VIP helps Veterans remain independent and self-sufficient in their home, there may be inadequate support for Veterans as their needs change and remaining at home is no longer an option.
- Eligibility criteria are often too complex and difficult for Veterans or their family members to understand.
- Different groups of Veterans are entitled to different levels or types of support and programs. Entitlement is often determined by type of service rather than need.
- It is unclear how VAC’s strategy for providing support links into the support provided by the Canadian Health Care system.
The report concludes that the demographic shift in the makeup of VAC’s client population has opened a unique window of opportunity to make changes to the continuum of care for injured Veterans. Consistent with the Gerontological Advisory Council’s reportFootnote 1, we have recommended seven changes that will help to reduce complexity and enhance benefits and services to those who need them, when and where they are needed, while ensuring that eligibility is not tied to a Veteran’s status or location of residence. Benefits and services should be flexible enough to move and adapt seamlessly with the Veteran as needs and care settings change.
The report makes the following recommendations:
- Recommendation 1
- Follow-up contact with Veterans Independence Program recipients should be made on at least an annual basis and more frequently for those at higher risk (with in-home assessments when necessary) to ensure timely and accurate identification of changing needs as Veterans age.
- Recommendation 2
- Eliminate the inconsistency in Veterans Independence Program eligibility for housekeeping and grounds maintenance for survivors and spouses so that they may all have access to the services they need, regardless of what the Veteran received or did not receive prior to their death or involuntary separation.
- Recommendation 3
- Adjust the eligibility criteria of the Caregiver Recognition Benefit to provide easier access to compensation for caregivers when service-related conditions inhibit a Veteran’s ability to perform Instrumental Activities of Daily Living and childcare.
- Recommendation 4
- Introduce additional financial support that can be used to subsidize assisted living options for Veterans whose needs do not require Long Term Care, but who cannot stay in their own homes.
- Recommendation 5
- Merge the Veterans Independence Program and Long Term Care program into one “Continuum of Care” program such that access is determined once, and criteria are transparent, understandable, and based on the physical and mental health needs of the Veteran.
- Recommendation 6
- Reduce the complexity of 28 different eligibility groups, currently using service type, such that access to continuum of care support is based on the physical and mental health needs of Veterans.
- Recommendation 7
- Develop and publicly communicate a strategy to ensure that the continuum of care needs of all Veterans are being met within the current context of the Canadian Health Care system.
Implementing these recommendations will make a positive difference by helping to ensure that ill or injured Veterans and their families receive the lifetime of care and support they need and deserve as a result of their service and sacrifice to Canada. We will continue to monitor VAC’s progress to ensure the best possible outcome for those who served.
Introduction
Access to adequate LTC for Veterans continues to be the subject of news reports across the country. This issue is not exclusive to the Veteran population. Canada’s population is aging at a rate that is accelerating, presenting the government with a larger group requiring improved LTC and access to that care. By 2036, seniors will represent 25% of Canada’s population. With the traditional war-service Veteran population declining and the overall CAF Veteran population aging, VAC needs to take into consideration the impact these demographic shifts will have on LTC requirements. Further, rates of obesity, mental health conditions and chronic pain, owing to higher rates of back problems and arthritis, have been found to be higher among Veterans than among the general population, and as such, even younger Veterans may require additional care and support.Footnote 2
Given the current environmental pressures to ensure adequate support for aging Veterans, and considering that 15% of all complaints received by the office relate to VIP and/or the LTC ProgramFootnote 3, the OVO conducted three reviews in 2013 and 2014. The first two reviews looked at the VIP and LTC Program, while the third review considered assisted living in the context of the continuum of care:
- Veterans Long Term Care Needs: A Review of the Support Provided by Veterans Affairs Canada through its Long Term Care Program (LTC review) (May 2013);
- Veterans’ Long Term Care Needs: A Review of the Support Provided by Veterans Affairs Canada through its Veterans Independence Program (VIP review) (December 2013); and
- Assisted Living in Canada: A Shelter and Care Option for Veterans (assisted living review) (February 2014).
Canada's population is aging at a rate that is accelerating
Together, the reviews provided insight to the challenges faced by Veterans and their ongoing needs from both a “continuum of care” and a program specific context. The concept of continuum of care involves “an integrated system of care that guides and tracks patients over time through a comprehensive array of health services spanning all levels of intensity of care.”Footnote 4 The reviews provided a picture of the continuum of care for Veterans and the array of supports available through both the VIP and LTC Program. In addition, other programs and benefits provide support for Veterans such as the Treatment Benefits Program, the Attendance Allowance, and the Family Caregiver Relief Benefit (FCRB) (depending on the applicable Act)Footnote 5.
The purpose of this report is to:
- Highlight the issues identified in the three initial reviews as well as in other research;
- Make recommendations to address gaps identified in the three care settings across the continuum of care: care at home, assisted living, and LTC;
- Provide an update within the evolving Canadian demographic context.
VAC has also begun work to examine their VIP and LTC programs, and a similar conversation is also happening in the broader society as Canada’s population ages. This report aims to contribute to this work by providing timely information and recommendations to address these issues for Canada’s Veterans.
Definition of Terms
The following section provides the definitions OVO has adopted when discussing health care and the different categories of “Veteran.”
Health Care Definitions
Most health care is provided to Canadians under the purview of Canada’s provinces and territories. Definitions of services, types, and levels of care vary by jurisdiction. VAC provides programs, services, and financial support to Veterans in all jurisdictions across Canada. Because each jurisdiction uses its own terminology, the meaning of the terms used in this report may not correspond to those in each province or territory.Footnote 6 The definitions below have been chosen and defined in a way that best describes VAC’s offerings and possible gaps therein.
Activities of Daily Living (ADLs): “Activities of daily living means self-administered care, including eating, dressing, washing/bathing, grooming, toileting, walking, etc.”Footnote 7
Assisted Living: The Canadian Centre for Elder Law defines assisted living as a setting that provides “additional personal assistance and services” when a client can no longer live comfortably in their own home.Footnote 8 This definition is broad enough to include all supportive housing facilities that would not offer the intensive care provided in LTC facilities. Thus, assisted living refers to care that combines housing with support, hospitality services, and potentially some health care. On the care continuum, assisted living generally falls between home care at the lower end of the assistance spectrum and LTC at the higher end. Assisted living facilities are typically for those who do not need the level of care provided by LTC facilities but are unable to stay home because they need help with daily living, such as laundry, transportation, meal preparations, medications, etc. Facilities differ in the type and range of services they offer.Footnote 9 In addition, services may come unbundled from the accommodation fees, on a fee for service basis, which distinguishes them from LTC facilities. They typically “emphasize resident autonomy and privacy in a homelike, congregate community setting.”Footnote 10
Continuum of Care: Continuum of care refers to “an integrated system of care that guides and tracks patients over time through a comprehensive array of health services spanning all levels of intensity of care.”Footnote 11 Generally, ‘continuum of care’ refers to the care offered in particular settings – from home care that aims to maximize independent living, to assisted living that provides additional supports and supervision, to LTC with more intensive services.
Instrumental Activities of Daily Living (IADLs): “Instrumental activities of daily living … are those activities which comprise a secondary level of tasks that are not essential to health or survival but which a person should be able to do in order to function independently. IADLs may include shopping, housekeeping, banking, errands, grounds maintenance, minor home repairs, and driving or taking public transportation”.Footnote 12
Long Term Care (LTC): Long term care refers to, “ongoing, indefinite, care for individuals who can no longer fully care for themselves”. It includes medical supervision, nursing care, personal care, housing support, and social programming.Footnote 13 In most cases, long term care patients do not require the acute care provided in a hospital setting, but they do require ongoing medical oversight and care that cannot be provided at home or in assisted living facilities. LTC includes both intermediate and chronic care.
Chronic Care: “…[A] service provided in a health care facility to meet … the need of a person for personal care and for diagnostic, nursing, and therapeutic services provided by a health professional on a continuing basis, where the person is chronically ill or has a functional disability and the acute phase of the illness or disability has ended, whether or not the status of the illness or disability is unstable…”Footnote 14 Most individuals in Canada who require chronic care would obtain that care while residing in a LTC facility.
Intermediate Care: “[A] service provided in a health care facility to meet … the need of a person for personal care on a continuing basis under the supervision of a health professional, where the person has a functional disability, has reached the apparent limit of recovery and has little need for diagnostic or therapeutic services ...”Footnote 15 Most individuals in Canada who require intermediate care would obtain that care while residing in a LTC facility.
Veteran Category Definitions
There are numerous Veteran categories identified in VAC’s legislation and regulations. One of the findings in previous OVO reports is that there are simply too many categories of Veterans leading to complex webs of eligibility for various programs depending on service history details, date of application, degree of service-related injury or illness, income level, and so on. While the legislation and regulations identify over 28 separate eligibility groups for LTC funding alone, in this report we will use the following terminology in the interest of clarity and simplicity. Note that the eligibility criteria are complex and these simplified categories will not accurately reflect every Veteran. For more information on Veteran categories and their corresponding eligibility, see the OVO’s LTC review, Annex 1 – Definition of Client Groups.Footnote 16
War Service Veterans: Served during WWII or the Korean War. Can access benefits through the Pension Act and the War Veterans Allowance Act.
Canadian Armed Forces (CAF) Veterans: Served any time after 1947, except during the Korean War. Veterans who applied for disability benefits prior to April 1, 2006 can access benefits through the Pension Act (if the application was approved). Veterans who applied for disability benefits after April 1, 2006 can apply for a different suite of benefits through the Canadian Forces Members and Veterans Re-establishment and Compensation Act (known as the New Veterans Charter (NVC)).Footnote 17
Pension Act Veterans: Veterans who have eligibility under the Pension Act.
New Veterans Charter Veterans: Veterans who have eligibility under the NVC.Footnote 18
Current Context
Canada’s population is aging. The Canadian Institute of Health Information (CIHI) noted, in their 2011 Annual Health Care report on seniors and aging, that there is a “demographic shift into an accelerated period of population aging”, and they forecast that seniors will account for 25% of the Canadian population by 2036. It is important to note that while we are seeing an increase in the number of people considered “seniors,” this group is living longer and remaining healthier than previous generations of the same age group.Footnote 19
Veteran Demographics
There are an estimated 670,100 Veterans in Canada. Some key details of that population are presented below (see footnotesFootnote 20,Footnote 21, Footnote 22,Footnote 23):
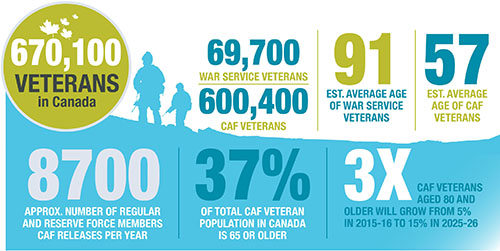
Veteran Demographics
There are an estimated 670,100 Veterans in Canada. Some key details of that population:
- There are an estimated 69,700 War Service Veterans and 600,400 CAF Veterans;
- The average age of War Service Veterans is 91;
- The average age of CAF Veterans is 57;
- The CAF releases approximately 8700 Regular and Reserve Force members per year;
- More than one-third (37%) of the total CAF Veteran population in Canada is 65 or older.
- The proportion of CAF Veterans aged 80 or older is expected to triple over the next decade, from 5% in 2015-16 to 15% in 2025-26.
Not all Veterans are VAC clients and they do not always become clients upon their release from the CAF. Over half of VAC’s yearly new intake clients have been released from the military for more than 15 years.Footnote 24
VAC forecasts that its client profile will change significantly by 2021 (see footnote Footnote 25):
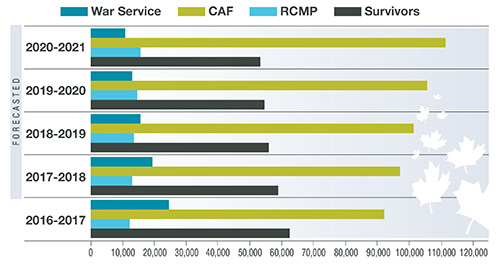
Infographic 2
The number of War Service Veterans being served by VAC is forecast to decrease from 24,300 in 2016-17 to 10,200 in 2020-21 while the number of CAF Veterans VAC serves is forecasted to increase from 92,600 to 110,200 during the same period. The total number of War Service and CAF Veterans being served by the Department will increase by 3,500, from 116,900 in 2016-17 to 120,400 in 2020-21.
VAC, however, predicts a decrease in the overall number of clients it will serve over the next 5 years, from 191,800 to 189,600.
Because the LTC Program is linked most often to War Service Veterans, the cadre of CAF Veterans eligible is dropping as the War Service Veteran population diminishes over time. CAF Veterans, however, may require continuum of care support as they age or as their injuries require. Given that the CAF intends to grow their enrollment to over 100,000 members, an increase in members being medically released is anticipated for future years.Footnote 26

Consequently, VAC’s VIP and LTC Program are both poised for large shifts in the composition of their client base. The impact on forecasts for programs is as follows:
- As of March 31, 2016, 56,095 Veterans received benefits through the VIP.
- By 2020, VAC forecasts this number will decrease to 47,100.Footnote 27
- In March 2016, there were 6,441 inpatient Veterans at LTC facilities.Footnote 28
- By March 2026, VAC forecasts only 2,329 Veterans in LTC facilities.Footnote 29
- Costs for the VIP are forecast to decrease from $352.6M in 2015-16 to $340.6M by 2023 (adjusted for inflation).Footnote 30
- LTC expenditures are expected to decrease from $314.7M to $183.9M between 2015-16 and 2020-21.Footnote 31
This decrease in LTC expenditure forecast presents a unique opportunity for VAC to renew their programming and better target funding to support positive results for Veterans and their families.
VAC’s Programs and Services
VAC’s three pillars of health and medical support programs are the:
- Treatment Benefits Program;
- VIP; and
- LTC Program.
Each of these programs addresses elements of health care needs that can arise as Veterans age or require greater levels of care. This section outlines the main program support offered by VAC and when and where an eligible Veteran can access that support across the continuum of care.Footnote 32
Care at Home
The Veterans Independence ProgramFootnote 33
The VIP was developed to help eligible clients stay in their own homes for as long as possible while maintaining their dignity and health. The program provides financial contributionsFootnote 34 for the following home care services:
- Grounds maintenance, such as lawn mowing and snow removal;
- Housekeeping tasks or domestic chores to assist with daily living (including laundry, grocery shopping, meal preparation, vacuuming, etc.);
- Personal care by a non-health professional to assist with such things as bathing, dressing and eating;
- Access to nutrition, such as Meals on Wheels;
- Health and support services by a health professional, such as nursing care, therapy, and personal care;
- Ambulatory health care, such as professional assessments, diagnostic services, and social and recreational services provided by a health professional as well as transportation to access these services;
- Transportation to foster independence and avoid social isolation (for War Service Veterans assessed as low income); and
- Home adaptations to the principal residence to enable the client to perform activities of daily living.Footnote 35
Since its establishment in 1981, when it focused on the provision of services to war service pensioners, the VIP has changed and expanded to meet the needs of other groups such as: those who qualify for a disability award, a War Veterans Allowance (or due to age and income are income-qualified), or have been the primary caregiver for an eligible Veteran or civilian.Footnote 36 Generally, the services provided are not already covered by the province or private insurance or are provided to augment those already in place but which are not meeting the needs of the individual. Of note, only two VIP service elements (housekeeping and/or grounds maintenance) are available to primary caregivers or survivors, not the full suite of VIP services.
Treatment Benefits
The Treatment Benefits Program includes 14 Programs of Choice: Aids for Daily Living; Ambulance/Medical Travel Services; Audio (Hearing) Services; Dental Services; Hospital Services; Medical Services; Medical Supplies; Nursing Services; Oxygen Therapy; Prescription Drugs; Prostheses and Orthoses; Related Health Services (includes services such as physiotherapy and psychological counselling); Special Equipment (can include items such as: home adaptation, home modifications, and mobility devices; and Vision (Eye) Care. It is important to note that not all Veterans are eligible for all Programs of Choice and eligibility criteria can be complex.
Attendance Allowance
The Attendance Allowance is a monthly allowance provided under the Pension Act and is only available to Veterans with a Disability Pension of 1% or more and/or Prisoner of War compensation.Footnote 37 The allowance provides funding if a Veteran is deemed totally disabled and is in need of attendance for activities such as feeding, bathing, dressing, toileting, mobility, and/or medical administration. The need does not have to be service related or related to the pensioned disability. The Attendance Allowance is payable regardless of where a Veteran lives. However, it will not usually be payable when a Veteran resides in a LTC facility unless a Veteran is in receipt of the allowance prior to being admitted to long term care, in which case they typically continue to receive it while in care.Footnote 38 The amount paid depends on the assessed need, which determines the Veteran’s grade, between 1 and 5. Monthly amounts range from $289.50 at Grade 5 to $1,808.74 at Grade 1.Footnote 39
Family Caregiver Relief Benefit / Caregiver Recognition BenefitFootnote 40
The Family Caregiver Relief Benefit (FCRB) was implemented in July 2015 to provide relief to informal caregivers of seriously injured NVC Veterans. The benefit is a tax-free grant of just over $7,000/year and is paid to the Veteran to ensure that they continue to get the support they need when their informal caregiver is temporarily unavailable. Budget 2017 announced the Caregiver Recognition Benefit (CRB) to replace the FCRB, effective April 2018. While few details have been released to date, the government has committed to providing $1,000/month to recognize informal caregivers, and this amount will be paid directly to the caregiver, rather than the Veteran and therefore requires the Veteran to designate and identify a caregiver.Footnote 41 A comprehensive review and evaluation of the FCRB and/or the CRB is outside of the scope of this report, however, the OVO is pleased that the government has developed this benefit in-line with a recommendation we made in 2013, given the importance of recognizing the vital role informal caregivers often play in maintaining the health and well-being of Veterans.Footnote 42
Care in Assisted Living
Veterans Independence ProgramFootnote 43
Veterans can access VIP home care benefits when they reside in an assisted living facility (which is considered their primary residence). Provision of services is needs-based, and services provided by the facility as part of their program are considered. If the spouse remains in the home, he or she may be eligible to receive VIP home care benefits based on their needs. The spouse is required to complete an application and can only receive the benefit (housekeeping and/or grounds maintenance) that was in place at the time the Veteran was admitted to the assisted living facility.
Treatment Benefits & Attendance Allowance
Veterans can continue to access Treatment Benefits and the Attendance Allowance (see above for details.)
Care in a Long Term Care Facility
Eligible Veterans in residential LTC facilities can access funding through VAC’s VIP-Intermediate Care (IC) or through the LTC Program.Footnote 44Typically, the cost of care in a LTC facility has two components: a medical component and an accommodation/meal component. Most of the medical component (nursing, physician oversight, diagnostic and therapeutic services, etc.) is covered under provincial health insurance plans and often no cost is borne by the client. The accommodation component (bed space and meals, often called a “co-payment”) is sometimes the responsibility of the patient and varies according to room type, income level, and province.
Long Term Care Program
Under the LTC Program, VAC provides funding for two types of care: intermediate care and chronic care.Footnote 45 Intermediate and/or chronic care may be provided in either contract or community beds:
- Contract beds are identified and funded for priority access by Veterans under federal-
provincial agreements and agreements with health authorities and specific institutions. Many are located in former federal Veterans’ facilities, with a smaller number in 197 provincially licensed facilities across Canada. - Community beds are beds in provincially licensed facilities that are not specifically identified and funded for Veterans and access to these beds is not prioritized for Veterans. Veterans are considered for placement based on health needs along with all residents of that province.
As of March 2016, there were 3,961 VAC clients in community beds and 2,480 (of 3,045 available) in contract beds.Footnote 46 Given the increasing number of vacant contract beds and demand to expand access to other groups of Veterans, discussions to expand access were initiated with provincial health authorities and senior administrators of what were previously Veterans hospitals. As a result, VAC launched a 2-year pilot that created a new bed type: “Preferred Admission” community beds. In June 2016, the Department began negotiating new arrangements for preferred admission to community beds for Veterans who are eligible for care in a community facility other than in a contract bed. These agreements are for a period of 2 years.Footnote 47
In general, Veterans in a LTC facility are required to contribute to a maximum monthly amount of $1,016.96 for their accommodation and meals, unless their need for care is directly attributable to their pensioned or awarded condition, or they are a War Service Veteran who has been deemed ‘seriously disabled’ (sum of disability assessments is 78% or higher) or if the Veteran has insufficient income.Footnote 48 The maximum amount is updated annually on October 1.Footnote 49
The LTC Program provides funds to Veterans to cover part or all of the accommodation component to a daily maximum of $252.02 for chronic care and $150.19 for intermediate care in a community setting. The level of care required is determined by a VAC Nursing Services Officer who either directly performs a nursing assessment or reviews a provincial assessment to determine care need.Footnote 50 VAC’s contribution for care in a contract bed is not determined on a per-diem basis because payment and service arrangements differ; in some cases VAC pays extra for priority access, in others it pays the full cost of operating the facility, and in others VAC pays for additional programs or services.
Veterans Independence Program: Intermediate Care in a Long Term Care Facility
Veterans who do not qualify for the LTC Program may be eligible for the VIP’s Intermediate Care Program (VIP-IC). VIP-IC provides funding for LTC in a community facility, other than a contract bed.Footnote 51
The maximum rate payable for VIP-IC is the same as for intermediate care in a community facility under the LTC Program: $150.19/day.Footnote 52 The rate payable by VAC is determined by the income of the Veteran. These rates are updated annually.
Treatment Benefits
Veterans can continue to access Treatment Benefits (see above for details).
Office of the Veterans Ombudsman Reviews
A Review of the Support Provided by Veterans Affairs Canada Through its Long-Term Care Program

The OVO conducted two reviews of VAC’s programs providing continuum of care assistance: the LTC Program and VIP. The reviews evaluated the programs using three criteria: eligibility, accessibility, and cost. The OVO also published a review exploring the option of assisted living for Veterans who find themselves not able to stay at home, but not yet ready for LTC.
The OVO’s review of the LTC Program in May 2013 found that complex eligibility is a significant issue for this program. Aside from eligibility concerns, accessibility is determined largely by provincial health authorities, which can create added complication. The review noted that VAC’s LTC expenditures are projected to decrease until at least 2021-22. This is explained by the attrition of the War Service Veteran population – the group with the greatest eligibility for the LTC Program.
Subsequently, the OVO’s December 2013 VIP review found the program to be cost-effective for the Department and that services are generally accessible for most clients.Footnote 53 The review, however, also found that, much like the LTC Program, eligibility for VIP benefits and services is complex and inflexible.
The February 2014 OVO review on assisted living did not examine an existing VAC program but rather considered assisted living options for Veterans; a commonly chosen alternative to home care support and LTC. The review found that because of long wait times for LTC beds, many are faced with the choice of moving to an expensive assisted living facility or staying in their own homes even when they require additional supports. This choice is not viable for many who cannot afford assisted living.
Findings and Recommendations across the Continuum of Care
When examining the needs of Veterans across the continuum of care, from home care to assisted living and/or long term care, previous OVO reviews show that VAC programs provide significant support. There are, however, gaps that remain. The following analysis looks at each stage of the continuum of care from care at home to assisted living and LTC. It describes the challenges with the current programs from the Veteran perspective, using a lens of fairness to determine whether adequate programs are in place to sufficiently meet the needs of Veterans and whether or not those programs are easily accessible. Where gaps are identified, recommendations are made which, if implemented, would help to ensure that VAC is providing the support that Veterans and their families need and deserve.
VAC programs provide significant support, there are, however, gaps that remain
Care at Home: Timely Follow-Up, Needs-Based Approach
The provision of care and support at home aims to maintain a person’s independence for as long as possible in a place where they are most comfortable. Home care can be provided by informal caregivers such as close family members, as well as by community service providers. VAC’s VIP was created specifically for this purpose.
The VIP provides needed home care services in a cost-effective manner, promoting client independence, well-being, and comfort. For instance, according to research commissioned by VAC and the Government of Ontario, due to the added expense of facility user-fees, clients living at home paid only a fraction of the expense associated with living in a facility: $5,372/year compared to $12,495/year in 2006.Footnote 54 The report also analyzed costs to government. For clients requiring the same level of care,Footnote 55 the cost to government of providing in-home services was substantially less than providing services through a facility: $14,581/year versus $64,594/year.Footnote 56
Care at home can also delay the age of admittance to a more costly assisted living facility or LTC bed, extending cost-effectiveness and giving Veterans the choice to remain at home longer. VAC has determined that Veterans who receive VIP home care services such as house-keeping, grounds maintenance, and/or personal care are on average 2.5 years older when they are admitted to a LTC facility, when compared with Veterans who did not receive VIP services at home. The average age of admittance for VIP clients is 92.7 years, whereas for non-VIP clients the average age is 88.6. Perhaps even more importantly, VAC reports that VIP clients live longer than non-VIP recipients: 92.7 years as compared with 92.2 years.Footnote 57 This reflects the available research indicating that home care is often an effective alternative to institutional care.Footnote 58
Follow up Contacts/Assessments
Despite the strength of the VIP’s home care program, concerns have been raised regarding the adequacy of VAC’s infrequent monitoring of VIP clients. A recent VAC evaluation of the program indicates that a new procedure was implemented to reduce the amount of follow-up with VIP clients. Previously, the department would contact recipients on a yearly basis to re-assess any changes in the need for services. In early 2015, this interval increased to three years with automatic renewals between follow-up contacts. The report notes that the lengthy intervals between contact makes it less likely that additional needs will be identified, and also increases the risk of overpayment if clients change residences without notifying the department.Footnote 59 This VIP follow-up contact is often the only contact an elderly Veteran will have with the department. VAC does not conduct regular assessments, or provide case management services as a matter of course, and does not do home visits with its elderly Veteran population. Given the frailty and changing needs of this population, more departmental contact and assessment would be beneficial. Follow‑up frequency should be increased to once per year for all VIP clients and include in‑home assessments as necessary.
Lengthy intervals between contact makes it less likely that additional needs will be identified
Recommendation 1: Follow-up contact with Veterans Independence Program recipients should be made on at least an annual basis and more frequently for those at higher risk (with in-home assessments when necessary) to ensure timely and accurate identification of changing needs as Veterans age.
Access to Housekeeping and Grounds Maintenance Services
The OVO’s VIP review of December 2013 highlighted an inconsistency in the Veterans Health Care Regulations (VHCR) regarding the eligibility of certain survivors/primary caregiversFootnote 60 for Housekeeping and Grounds Maintenance Services:
- If a Veteran received both services, the survivor/primary caregiver can keep both upon the death of the Veteran as per Section 16 of the VHCR.
- If a Veteran received only one of the two services, the survivor/primary caregiver is only eligible for that service after the death of the Veteran.
- However, in 2008, the VHCRs were amended to provide greater access to continuation of VIP services, but only for income-qualified survivors (or those in receipt of the disability tax credit) of War Service Veterans. For this specific sub-group of survivors, if the Veteran did not receive either service, the survivor can apply for and potentially receive both services upon the death of the Veteran.Footnote 61
It is difficult to understand why a survivor/primary caregiver receiving one VIP service at the time of the Veteran’s death would be denied access to the other service while a survivor who had none of the services can apply and receive both services after the Veteran’s death. Furthermore, this expanded eligibility is limited only to survivors of Veterans of the Second World War and the Korean War. Most importantly, access to VIP services should be based solely on needs, not on the nature of Veterans’ military service and whether or not they were in receipt of housekeeping or grounds maintenance services prior to their death.
A further issue that is often brought to our attention is an unfairness for spouses who were involuntarily separated from the Veteran for medical reasons (for example, when the Veteran moves to the residence of an adult child but the spouse stays in the home). In these cases, the Veteran can retain eligibility for housekeeping grants at the new residence, but the spouse loses the benefit for the family home. We have had several cases come to our office where the spouse struggled to take over these responsibilities after the Veteran had left and taken the grant with him or her.
Recommendation 2: Eliminate the inconsistency in Veterans Independence Program eligibility for housekeeping and grounds maintenance for survivors and spouses so that they may all have access to the services they need, regardless of what the Veteran received or did not receive prior to their death or involuntary separation.
Adequate Support for Instrumental Activities of Daily Living
From OVO town hall meetings to complaints received by our frontline, Veterans have voiced concerns that VAC is not doing enough to recognize and compensate for service related physical and/or mental health conditions that limit their ability to perform IADLs (such as grocery shopping, errands, meal preparation, housekeeping, laundry, lawn maintenance, child care, preparation of children’ lunches, driving, banking, planning, keeping track of medical appointments, and providing psychological support), and as a result, they feel like they are an added burden when these activities often become the responsibility of a spouse or other informal caregiver. The complaint is understandable given shifts in family structure and gender roles, such as the fact that women make up an increasing proportion of the workforce.Footnote 62 Childcare, eldercare, and domestic responsibilities, which were traditionally the responsibility of the stay-at-home wife, are increasingly viewed as work that should be shared equitably.Footnote 63 An informal caregiver may have to take on the bulk of day-to-day tasks when a Veteran returns from service with physical and mental injuries. Given contemporary family structures, these added tasks are often in addition to full time work and eldercare responsibilities.
Currently, the VIP provides grants and reimbursements for costs associated with IADLs such as meal preparation, housekeeping, and grounds maintenance. However, in addition to meeting the war service, residency, and disability eligibility criteria, Veterans must also demonstrate that the services are not being provided by someone in the home. VAC’s Client Relatives (VIP) Policy states that, “VIP services are not intended to replace those provided by relatives …”, and the client will be deemed eligible only when an assessment of the capabilities and willingness of a live-in relative indicates that the client will go without the services if not approved.Footnote 64 In order to determine a client’s need for VIP services, VAC asks a series of “Guiding Questions for Determination of Need”.Footnote 65 Questions include (among others): With whom do you live? Are the individuals living with you willing and able to perform housekeeping and grounds maintenance activities around your home? Who typically prepares your meals? Are you or the person/people living with you able to drive, and if so, do you or the person/people living with you have access to a vehicle? Do you receive help with housekeeping or grounds maintenance activities, and if so, who assists you?
While provisions are made for situations where a live-in relative is or becomes unable to do this work, or (exceptionally) where the relative has too many other obligations, for the most part, if a relative will do this work in the absence of VIP services, VIP services will not be approved. Rather than recognizing the origin of the disability in service, and therefore covering what would normally be the Veteran’s share of these tasks had the disability not occurred, VAC has decided that an informal caregiver should take on this added burden.
In July 2015, VAC implemented a new benefit, the FCRB. To be eligible for this benefit, a Veteran must require one of the following:
- A level of care and supervision consistent with admission to an institution;
- Daily physical assistance of another person for most activities of daily living;
- Ongoing direction and supervision during the performance of most activities of daily living;
- Daily supervision and is not considered to be safe when left alone (i.e. Veteran poses a risk to him/herself or others if not supervised on a daily basis).Footnote 66
With the announcement of the CRB, the government has an opportunity to broaden eligibility and ensure that all significant caregiving activities are adequately recognized
The FCRB, however, does not provide assistance for IADLs. Similarly, for Pension Act Veterans, the Attendance Allowance can provide funding when an eligible Veteran needs help with their ADLs (for example bathing, dressing etc.), but does not include assistance for IADLs.
The burden to provide the IADLs has often been borne by informal caregivers who are not currently eligible for the VAC programs which should provide them with compensation and/or relief. With the announcement of the Budget 2017 CRB, however, the government has an opportunity to broaden eligibility for NVC Veterans to ensure that all significant caregiving activities are adequately recognized.
Recommendation 3: Adjust the eligibility criteria of the Caregiver Recognition Benefit to provide easier access to compensation for caregivers when service-related conditions inhibit a Veteran’s ability to perform Instrumental Activities of Daily Living and childcare.
Assisted Living: Bridge the Gap between Home Care and Long Term Care
Both the OVO’s assisted living review and VAC’s joint report with the Government of OntarioFootnote 67 found that assisted living can be cost-effective for governments when compared to LTC housing. The OVO’s review notes that the savings to government could be as much as $25-30,000 a year per person and suggests that this should be a strong incentive for VAC to fund assisted living for Veterans. Recognizing that assisted living can be cost-prohibitive to some individuals, but cost-saving to governments, many provinces offer subsidized assisted living arrangements.Footnote 68 Subsidized assisted living care is not universal across Canada. When assisted living care is subsidized, generally accommodation costs are solely the responsibility of the resident, with health support services paid for, in whole or in part, by regional health authorities. However, in cases where the province does not subsidize an individual’s assisted living care, the costs are borne entirely by the individual.
Pension Act Veterans in Assisted Living
The amount of support provided to Veterans in assisted living varies. Veterans with a Disability Pension can apply for and receive the Attendance Allowance while residing in an assisted living facility. An assessment for the Attendance Allowance will assign a grade level determining the non-taxable monthly amount. The maximum rate for the Attendance Allowance is $21,704.88/year.Footnote 69 The Veteran is not required to obtain and submit receipts, therefore the amount can go towards any expense chosen by the Veteran. Veterans can also continue to access VIP services; however, reimbursement of Personal Care expenses is limited to 59 days/year when a Veteran receives the Attendance Allowance.Footnote 70
NVC Veterans in Assisted Living
CAF Veterans with disability benefits under the NVC but no pension under the Pension Act are not eligible to receive the Attendance Allowance.Footnote 71 NVC Veterans can access some elements of the VIP while in an assisted living facility. The maximum rate for home care benefits under the VIP is $10,720/year,Footnote 72 however, this amount is substantially lower than the maximum rate of the Attendance Allowance ($21,704.88/year). Moreover, because Pension Act Veterans are also eligible for VIP home care benefits, VAC’s contribution to their care in assisted living can be substantially higher than VAC’s contribution to the care of NVC Veterans.
In order for VAC to continue to provide funding for services available under the VIP program while a Veteran resides in an assisted living facility, the following is required:
- A current client assessment identifying a need for the service provided;Footnote 73
- The duration and cost of the service is identified on an individual basis; and
- The cost of the service is equal to or less than the standard rate for similar services in the area.
Meal costs, for example, can only be claimed if a Veteran is charged for transportation to a location where a meal is provided, or for meal delivery.Footnote 74 These requirements can be onerous as it can sometimes be difficult to separate, for example, the costs of residence from the costs of personal care or meal costs. Additionally, if Veterans wish to be reimbursed for their personal care or meal costs, they must submit receipts. Furthermore, these benefits, including those that are grant-based, will not go as far as they would if the Veteran lived at home because assisted living is much more expensive.
Whether or not the new CRB will be available when a client resides in assisted living remains to be determined. At the time of this report, the policies for this new benefit have yet to be released. We know that the current FCRB is restrictive in this regard; if a Veteran “…resides in a health care facility wherein the level of care provided eliminates the need for an informal caregiver…” they are no longer eligible for the benefit.Footnote 75 Thus, if a Veteran has an informal caregiver while residing in Assisted Living, it is unlikely they will be eligible for the benefit.
Veterans without an informal caregiver have a greater need for institutional care, and sometimes this care is most appropriately provided in an assisted living facility
Veterans without an informal caregiver have a greater need for institutional care, and sometimes this care is most appropriately provided in an assisted living facility rather than LTC. One of the main reasons Veterans choose assisted living is due to the lack of informal caregiver support while living at home.Footnote 76 However, according to recent research, informal caregiving will decline as the number of senior citizens age. This is due to a variety of factors such as the migration of youth from rural areas to urban areas for education and employment; the decline of the nuclear family and smaller family sizes; and women’s increasing participation in the labour market.Footnote 77 Thus, Veterans may have an increased need for assisted living support if this decline in informal caregiving continues as forecasted. However, because NVC Veterans are not eligible for the Attendance Allowance, they receive less financial support from VAC that can be applied to assisted living costs. This gap in financial support can potentially create an incentive for NVC Veterans (like other Canadian seniors) to seek better subsidized care in a LTC facility. Moreover, recent research shows that Veterans, when compared to the general Canadian population, have a significantly higher prevalence of activity limitations at home.Footnote 78 Without an informal caregiver, Veterans may have a greater need than other Canadians for institutional support.
Patients can wait months - sometimes over a year - in a hospital until an adequate LTC bed becomes available
Because individuals may be referred to LTC facilities earlier than they would with greater support, either at home or in an assisted living facility, an increase in the competition for LTC beds can occur and place pressure on the entire health care system. Research in Ontario has demonstrated that, “an inability to perform instrumental activities of daily living ... such as preparing meals or using transportation or the telephone – remains a key driver of referral to residential LTC.”Footnote 79 This push towards LTC affects the entire system, including longer wait times for all. The Canadian Medical Association connects lengthy hospital wait times with inappropriate placement of individuals whose condition is stable, but who are not provided with home or community support. Patients can wait months – sometimes over a year – in a hospital until an adequate bed in a LTC facility becomes available. These seniors include Veterans who wait along with their fellow Canadians.Footnote 80
In June 2016 the OVO recommended that a strategy be developed wherein VAC reinstate funding for an assisted living option.Footnote 81 VAC previously had a program to provide funding in this area, but as part of a program review in the 1990s, funding for adult residential care beds was eliminated in 1995 and not replaced.Footnote 82 As part of the review, it was recommended that VAC analyze options for addressing this gap but this recommendation was never actioned. The Gerontological Advisory Council also highlights this lack of funding despite the fact that these facilities are often the most suitable housing and care option.Footnote 83 The Council stresses that this funding gap causes a ‘financial disincentive for Veterans to choose assisted living’ resulting in higher costs for the department and services that are less likely to meet the needs of the Veteran since they may be pushed into LTC before it is necessary. It would be more appropriate, the report states, if services and supports were not dependent on location, but rather on need, thereby giving Veterans more choice and better care, while also potentially saving the department money.Footnote 84 According to an internal VAC LTC review, 1 in 4 Veterans transition to an assisted living facility prior to entering LTC.Footnote 85 It is not known what, if any, support was received from VAC while they resided in assisted living. However, we do know that for NVC Veterans without eligibility for Attendance Allowance, the major cost burden falls to the Veteran. The sufficiency of the grades and amount of Attendance Allowance is outside of the scope of this report;Footnote 86 however, one of the strengths of the Allowance is that it is granted based on assessed need, rather than place of residence, thus providing the recipient with greater autonomy to choose where to live and from whom the care is obtained.
Recommendation 4: Introduce additional financial support that can be used to subsidize assisted living options for Veterans whose needs do not require Long Term Care, but who cannot stay in their own homes.
Accessing Care: Complex, Inflexible, and Inequitable Eligibility Criteria
Clear and simple eligibility criteria are important. Eligibility criteria can either open up or limit access to the support that Veterans need across the entire continuum of care. The OVO’s Reviews of VIP and LTC, however, found that the eligibility criteria for both programs are too complex, inflexible, and, because eligibility is often determined by a Veteran’s service type rather than need, inequitable.
Veterans Independence Program
The VIP review highlighted that, to be eligible for VIP, applicants have to meet strict criteria that could include service eligibility, minimum service requirements, service in specific wars or time frames, affiliation with particular organizations or military units, receipt of a certain pension, frail assessment, income qualification, or prisoner of war status. The review identified that the significant impact of that complexity was the time and expertise required for VAC staff to determine eligibility and the difficulty potential applicants have trying to determine if they are eligible, and if yes, to what components of the program.
Additionally, the review highlights the inflexibility of the eligibility requirements. This lack of flexibility has, in part, led to the creation of new policies to enable access for clients who would not otherwise be eligible.Footnote 87 Of note is the Frail Policy, which was introduced in 2003 as an internal directive giving staff authority to approve funding for VIP services based on need if the Veteran meets the “frail criteria”:
Frail is defined as the occurrence of a critical mass of physiological conditions that place an individual at risk for falls, injuries, illnesses or the need for supervision or hospitalization. Frailty also results in a severe and prolonged impairment of function with little or no likelihood of improvement. The designation of “frail” is based on the premise that for individuals suffering from multiple health conditions, one of which is the condition(s) for which entitlement to the pension/award was granted; this complex interplay of disabilities impairs their ability to remain self-sufficient at their principal residence.Footnote 88
This directive allows War Service and CAF Veterans with a disability pension or award to receive VIP services if they are ‘frail’, despite there being no direct relationship between the pensioned or awarded condition and their need for care. If a Veteran is eligible for VIP services under the frail criteria, they are also eligible for VIP-IC in a LTC facility.
Long Term Care
The OVO’s LTC review also identified complexity in LTC eligibility as an issue. LTC eligibility is twofold:
- As LTC is a health care service that falls under provincial jurisdiction, Veterans must first meet the eligibility criteria for LTC set by the province in which they reside.
- Once provincial eligibility has been established, a Veteran may apply to VAC for federal funding support.
Dealing with 28 separate eligibility groups is perhaps the most obvious source of complexity
VAC eligibility is largely based on four core criteria: type of military service, location of service, income (applies to War Service Veterans), and whether need for long term care is linked to a pensioned/awarded condition/illness. The OVO’s review identified 15 distinct client groups with different eligibilities to LTC benefits. Adding the various categories of eligibility for VIP-IC increases this number to 28 distinct client groups.Footnote 89
Dealing with 28 separate eligibility groups is perhaps the most obvious source of the complexity associated with VAC’s VIP and LTC programs. The need for so many groups is questionable considering that four eligibility categories account for 81% of all War Service Veterans in receipt of LTC support:
- Pensioner with non-pensioned condition,
- Income qualified Veteran,
- Frail pensioner, and
- Overseas Service Veteran.Footnote 90
To add to the complexity, eligibility also determines what type of bed (contract or community), whether any funding will be provided by VAC, and at what level. For example a War Service Veteran with a war-related disability pension is eligible for either intermediate or chronic care in a contract bed. In contrast, unless a CAF Veteran can access VIP-IC under the “Frail Policy”, he or she would only be entitled to VAC funding for a community bed, and only if the reason for being admitted to the facility was due to a service-related condition. The Frail Policy functions as a work-around to provide VIP-IC services, including intermediate care, for those who would not normally be eligible.
Determining whether a Veteran is eligible for LTC support in a contract bed can be a multi-step process involving at least four pieces of legislation and regulations: the Veterans Health Care Regulations, the Pension Act, War Veterans Allowance Act, and Veterans Benefit Act.Footnote 91
Complexity in eligibility makes it very difficult and time consuming for VAC staff to make eligibility determinations. As VAC’s internal LTC ReviewFootnote 92 highlights, there were 2,496Footnote 93 LTC eligibility decisions in 2015-16 and for each of those decisions, a number of documents add to the complexity:

Complexity:
- 32 program policies describing the eligibilities of various groups;
- 17 page Service Eligibility Guide
- 5 business processes
- 44 page user manual for RCSS;
- 8 directives;
- 4 page Eligibility and Payment Guide and a Maximum Rates Payable table;
- 5 Training guides on payment processing;
- 4 forms;
Merging the Veterans Independence Program and the Long Term Care Program
The complexity of each of the programs separate and distinct eligibility criteria makes it nearly impossible for a Veteran (or family member) to determine or understand their entitlement to benefits. Eligibility criteria determine entitlement to the VIP and/or LTC in general, but additional and varying criteria also determine entitlement to various components of the programs (for example, access to the Housekeeping Grant, VIP-IC, LTC contract vs. community bed, etc.). This difficulty is further exacerbated by often poor communication from VAC on what services the programs offer and to whom. On VAC’s external website, there is limited information about the components of the VIP or LTC and the eligibility and entitlements for each of the components. Even with access to the policies, there is no clear and simple guide to be able to quickly determine eligibility. Furthermore, some clients have multiple eligibility gateways if they have more than one service type (for instance, Military Service Pensioner and Special Duty Service Pensioner). Indeed, streamlining service delivery in order to provide a “single coordinated entry system” is cited as one of the 10 best practices for any continuum of care model.Footnote 94
Recommendation 5: Merge the Veterans Independence Program and Long Term Care program into one “Continuum of Care” program such that access is determined once, and criteria are transparent, understandable, and based on the physical and mental health needs of the Veteran.
Inequitable Long Term Care Eligibility Criteria
Not all Veterans are eligible for the same benefits. Some benefits require a link between the need for the benefit and a service-related injury. For example, former CAF members do not have the same access to the LTC Program as War Service Veterans, irrespective of whether the need is service-related. Veterans of WWII, and/or the Korean War have greater eligibility to the LTC Program, which includes higher levels of funding for chronic care than the VIP-IC Program.Footnote 95 As shown in the table below, Veteran Service Type is not determined by age, and many CAF Veterans are at or approaching an age where they are likely to require additional services and care.
| Veterans (VAC Clients) by Service Type and AgeFootnote 96 | ||
|---|---|---|
| Age | War Service | CAF |
| 60-69 | 0 | 14,256 |
| 70-79 | 106 | 17,439 |
| 80-89 | 3745 | 12,287 |
| 90+ | 21,165 | 704 |
| Total | 25,016 | 44,686 |
While CAF Veterans who are not War Service Veterans (including NVC Veterans), can access the LTC Program, their only gateway is a service-related injury that caused the need for admission to a LTC facility.Footnote 97 In contrast, for War Service Veterans who may be similar in age to non-war service Veterans, provisions are made for income qualification, in some cases where no service relationship exists between the need for LTC and the pensioned condition.
VAC indicates that over 90% of CAF Veterans accessing LTC support do so through VIP-IC via the Frail Policy. Without the Frail Policy, the majority of CAF Veterans would not have access to VAC support for a community bed (through VIP-IC) due to the LTC Program’s rigid eligibility criteria requiring a direct link between need and a pensioned or awarded service-related injury for CAF Veterans.
| LTC Inpatients by Eligibility Footnote 98 | ||
|---|---|---|
| Eligibility | War Service | CAF |
| Frail | 735 | 643 |
| Other | 4214 | 138 |
| Total | 4949 | 781 |
| % Frail | 15% | 82% |
Separating the effects of aging from service-related injuries and disabilities is often not possible. The Gerontological Advisory Council’s report states that service-related injuries can cause latent long term health effects, even when one appears healthy in the early stages of the condition.Footnote 99 Recent research confirms that the Veteran population experiences a significantly higher (10% or more) rate of arthritis, which can lead to osteoarthritis later in life, back problems, and chronic pain than the general Canadian population.Footnote 100 The report asserts that, “as Veterans age, it becomes virtually impossible – and unnecessary – to determine whether any functional decline or loss of independence is due to aging, military service or a combination of the two.”Footnote 101 In many of the cases that come to our office, the cause of an injury or illness like osteoarthritis is often not immediately obvious, particularly when the symptoms do not emerge until years later.
While access to LTC funding under the Frail Policy is important, the maximum rate payable is substantially less ($150.19/day) than the maximum rate payable under the LTC Program ($252.02/day). This discrepancy is problematic when we consider the difficulty of separating service-related conditions from normal aging. For instance, consider a Veteran who has a disability award for arthritis, who requires ‘chronic care’ in a LTC facility. If this condition is not the primary cause of their need to be admitted to a LTC facility, they will not qualify for the LTC Program, but could receive funding for VIP-IC under the ‘frail policy’. It is unclear, however, how a determination can be made that this debilitating service-related condition – arthritis – is not one of the main contributing factors leading the Veteran to require more intensive care (chronic) sooner than if he did not have the service-related condition.
Recommendation 6: Reduce the complexity of 28 different eligibility groups, currently using service type, such that access to continuum of care support is based on the physical and mental health needs of Veterans.
Veterans’ Access to Care in the Canadian Context
In September 2016, the Canadian Medical Association (CMA) released a report entitled “The State of Seniors Health Care in Canada”. Canada is facing an aging population that will strain the healthcare system. Because the health of seniors is the responsibility of the provinces, there are no national standards for types of care or access to care, leading to inequities between residents of different provinces and territories, as well as between urban and rural residents. Provinces have different fiscal capacities; broad economic changes affect each province’s economy differently. CMA’s report cites research indicating that a large majority of Canadians want a national senior’s strategy to “address needs along the full continuum of care”.Footnote 102
VAC’s 2017 internal LTC review notes that the “availability of provincially insured beds is decreasing” with the result that Veterans will face increasing competition to access community beds.Footnote 103 Provinces are not required to fund LTC; it is not included in the Canada Health Act as an insured service, meaning that provinces do not need to ensure LTC is universally accessible. Each province determines who is eligible for coverage, how much coverage is available, how much each individual must pay, and what they include in their plans.Footnote 104 For instance, the cost to the LTC client can range from $0/month in Nunavut where the government pays the entire cost – up to $3,437.09/month in New Brunswick.Footnote 105
Thus, accessibility to health care services on the continuum of care is often dependent on the resources provided by the province of residence and geographic location within that province (i.e. rural or urban). Veterans should not be treated less equally, or have less access to care, than other Canadians or other Veterans simply because of their location, their economic situation, and/or the resources available in their province or territory. Within the Canadian context, VAC must clearly identify where they intend to provide continuum of care support to Veterans who don’t necessarily have a service-related entitlement to LTC.
The ability to pay, or find a facility that will respect cultural differences or provide services in your first language are cited as the main barriers to adequate long term care for all Canadians.Footnote 106 These inequities are more or less pronounced depending on geographic location and the resources provided by the province or territory. In order for the Government of Canada to ensure that Veterans have equitable access to care across the country, consistent standards of care, access, and co-payment amounts are required in the absence of comprehensive coverage for all Veterans.Footnote 107
Recommendation 7: Develop and publicly communicate a strategy to ensure that the continuum of care needs of all Veterans are being met within the current context of the Canadian Health Care system.
Conclusion
There is a demographic shift in the makeup of VAC’s client population, and as a result, there is a unique opportunity to make changes to the continuum of care for ill or injured Veterans. Consistent with the Gerontological Advisory Council’s report,Footnote 108 changes are needed to ensure services are available when and where a Veteran requires them and are not tied to a Veteran’s status or location of residence. Benefits and services should be flexible enough to move and adapt seamlessly with the Veteran as needs and care settings change.
VAC has made a commitment to review the LTC/VIP Programs, and we hope that they will address the recommendations in this report as they complete this work. Doing so will help them reduce complexity and enhance benefits and services to those who need them. We will continue to monitor VAC’s progress to ensure the best possible outcome for those who served.